Eye Diseases
What Is Photophobia Light Sensitivity? Photophobia light sensitivity is a condition where bright lights hurt the eyes. It can range from minor irritation to a serious medical emergency. Mild cases may involve squinting in a brightly lit room, either inside or outside....
Eye Diseases
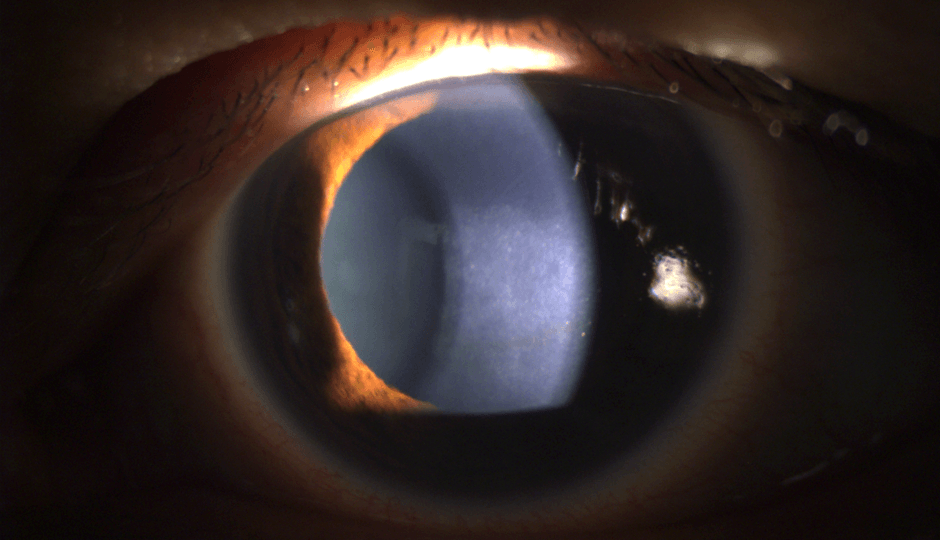
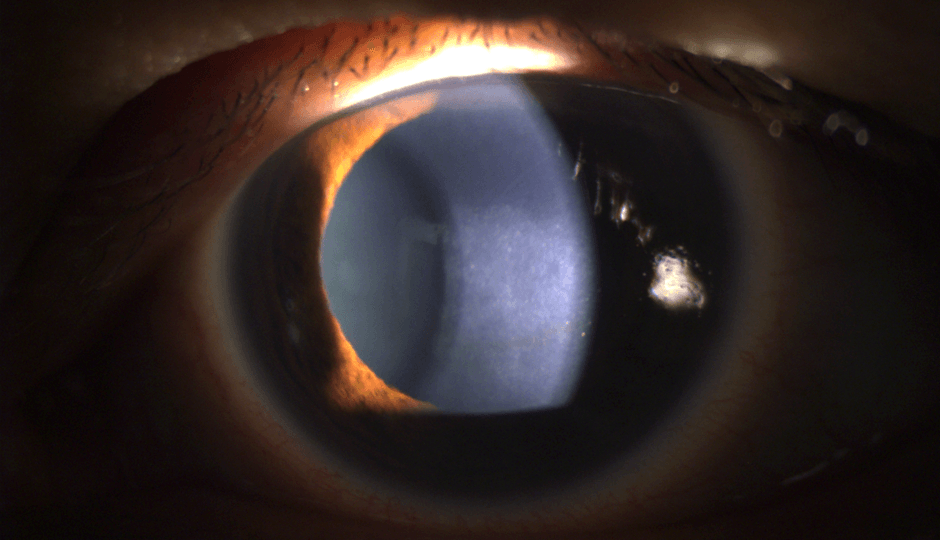
What Is Fuchs’ Dystrophy? Fuchs’ Dystrophy or Fuchs’ Corneal Endothelial Dystrophy (FECD) is an eye disease where the cells that line the inner surface of the cornea begin to slowly start dying off. It usually affects both of the eyes, and symptoms can include eye...
Eye Diseases
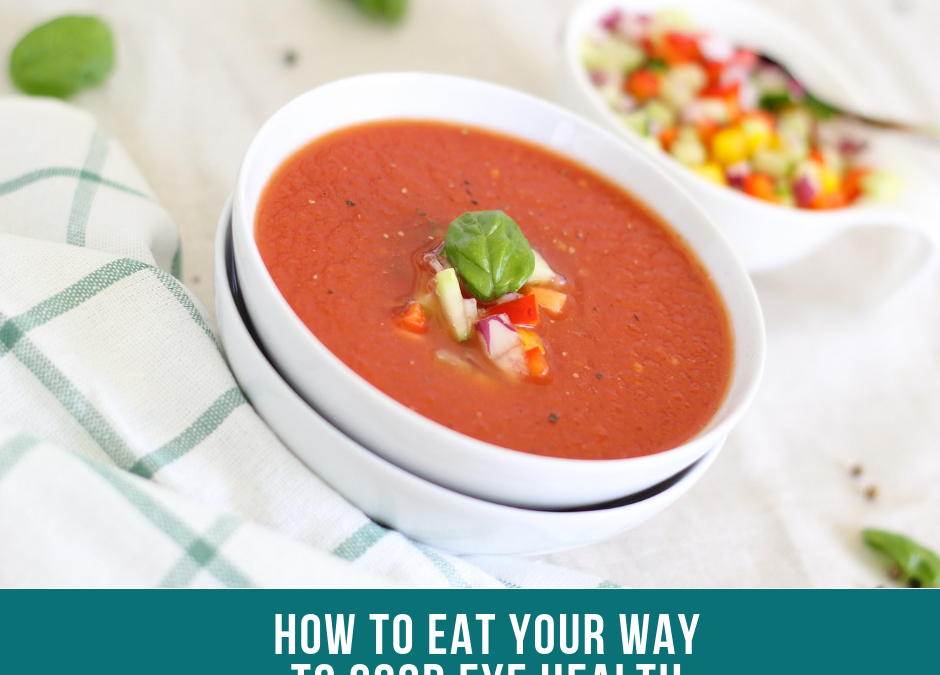
Anyone looking to improve their eye health, should start with examining their daily diet and lifestyle choices. New figures revealed by the Macular Society show that nearly 1.5m people in the UK are affected by macular disease – the nation’s biggest cause...
Eye Diseases
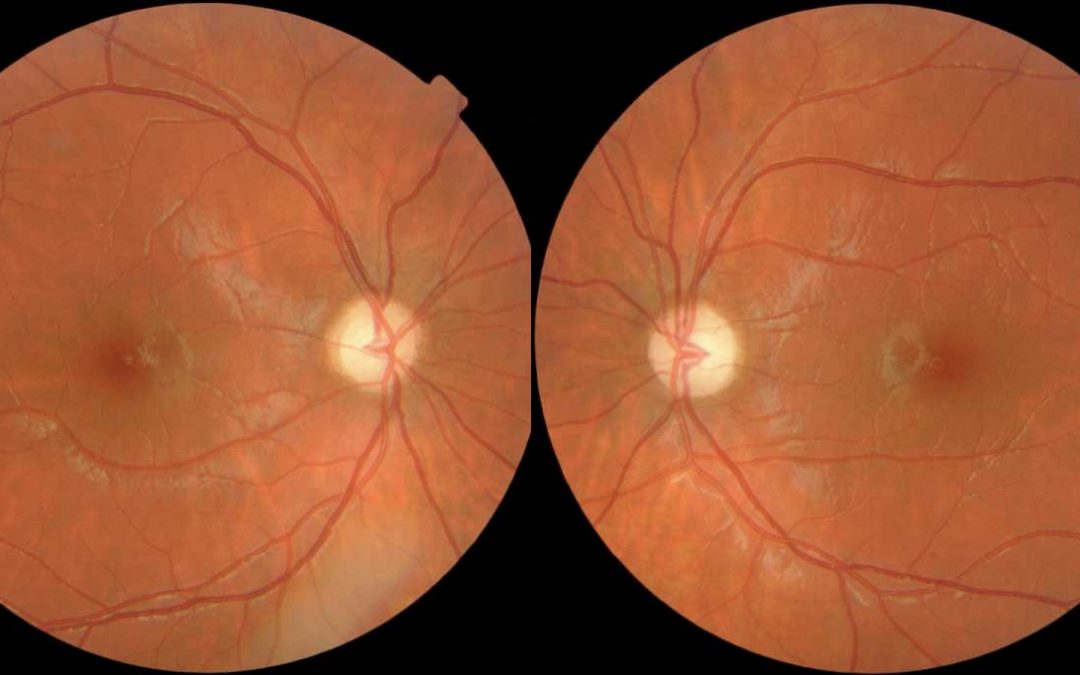
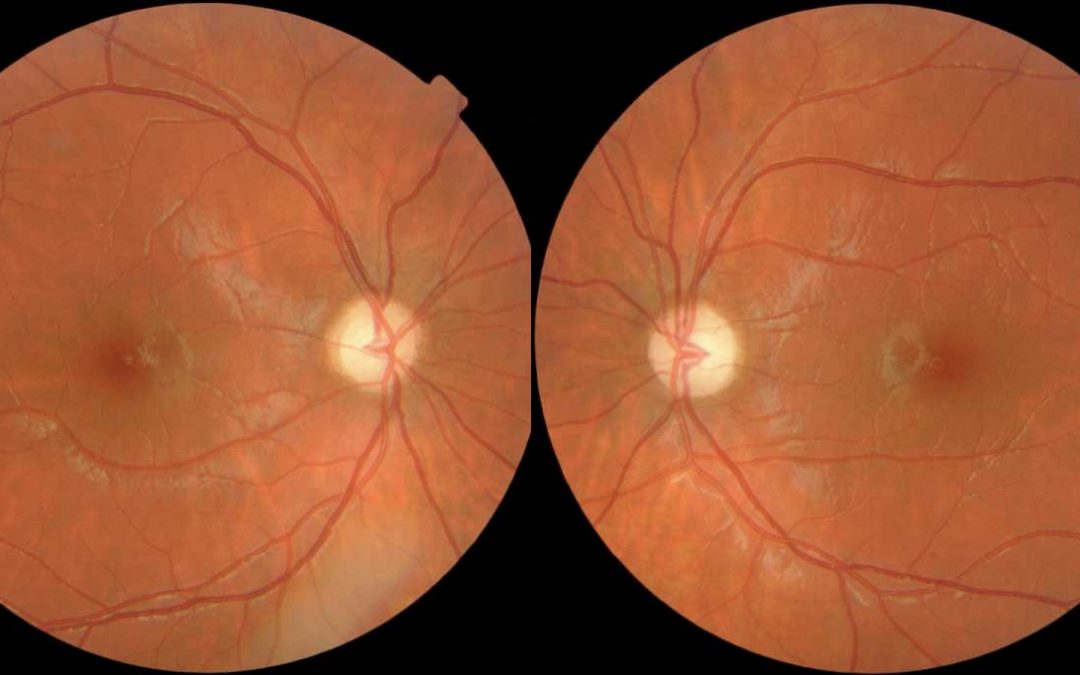
Juvenile Macular Degeneration – (see Macular Degeneration for overview). Macular degeneration is now being detected in children. This may be genetic or as a result of the poor diet of the mother during pregnancy or of the child (some children only eat vegetables...